99 problems...part 2
So, there you are having to decide how to treat before you have all the information you need. A bit of local knowledge and a close look at the horse will get you in the ballpark (see 99 problems...part 1). How do you take that first step?
Begin appropriate empiric treatment before going to
narrow spectrum
It may take between 24 and 72 hours (plus transportation
time and non-working days because some people have weekends) to obtain positive
identification of the pathogen. While you are waiting, broad-spectrum therapy can
begin. In horses, the combination of a beta-lactam like penicillin or
ampicillin with an aminoglycoside, whether it be amikacin in foals or
gentamicin in adults, is widely practiced with good reason. This will likely
cover most common bacterial infectious agents. Alternatively, other broad spectrum
antibacterials can be used. Knowledge of regional sensitivity and resistance
patterns, gained from previous culture results, is invaluable to minimize
chances of delaying effective therapy.
Once identification and sensitivity patterns (which antimicrobials
are effective in laboratory testing) of the organism are known, narrow spectrum
antimicrobials, when appropriate, can be initiated. Consideration should be
given to cost, the potential for toxicity in the current situation, and
potential to promote resistance in the population. Indiscriminate antimicrobial
usage has painted all medicine into a corner. This is nature at work: bacterial
resistance is promoted, and they will survive.
Have realistic expectations of the chosen agent
Treatment is more likely to succeed in an otherwise healthy
horse versus an immunocompromised horse or neonate. Antimicrobial treatment is
no substitute for considering the horse as a whole and providing the supportive
care necessary. If the horse can’t breathe or is dying from dehydration it is
time to address what will kill the patient first.
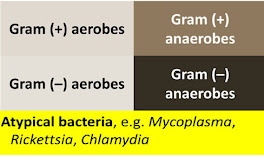
Some bacteria are inherently resistant to certain
antimicrobials making them ineffective. Identification of the organism allows
it to be categorized as shown. A particular antimicrobial may not be effective
in all categories, but this may not matter once the bacteria is identified. If
infection is mixed combination therapy may allow complete coverage.
Even if likely effective, the antimicrobial must be present
at the site of infection at a sufficient concentration for a sufficient time to
be successful. Can the antimicrobial penetrate
to the site of infection, and will it work in the conditions that exist? If fluid
is present in the pleural space (pleuritis) there is a high probability that a
very low oxygen environment exists within that fluid. This presents two
problems: not all antimicrobials will be able to penetrate fully into the
fluid, and conditions may not be favorable for their action even if they do. For
example, aminoglycosides require oxygen to be effective, so they should be
paired with a beta-lactam that is more likely to work in that environment as
this will increase the range of organisms covered.
In a few weeks I’ll talk about how a laboratory can guide
you through all of the above and help you make better treatment decisions.
Comments
Post a Comment